
Community care for our tiniest patients
During an uncertain time, a local mom and her newborn son found reassurance and specialized care in our hospital’s NICU
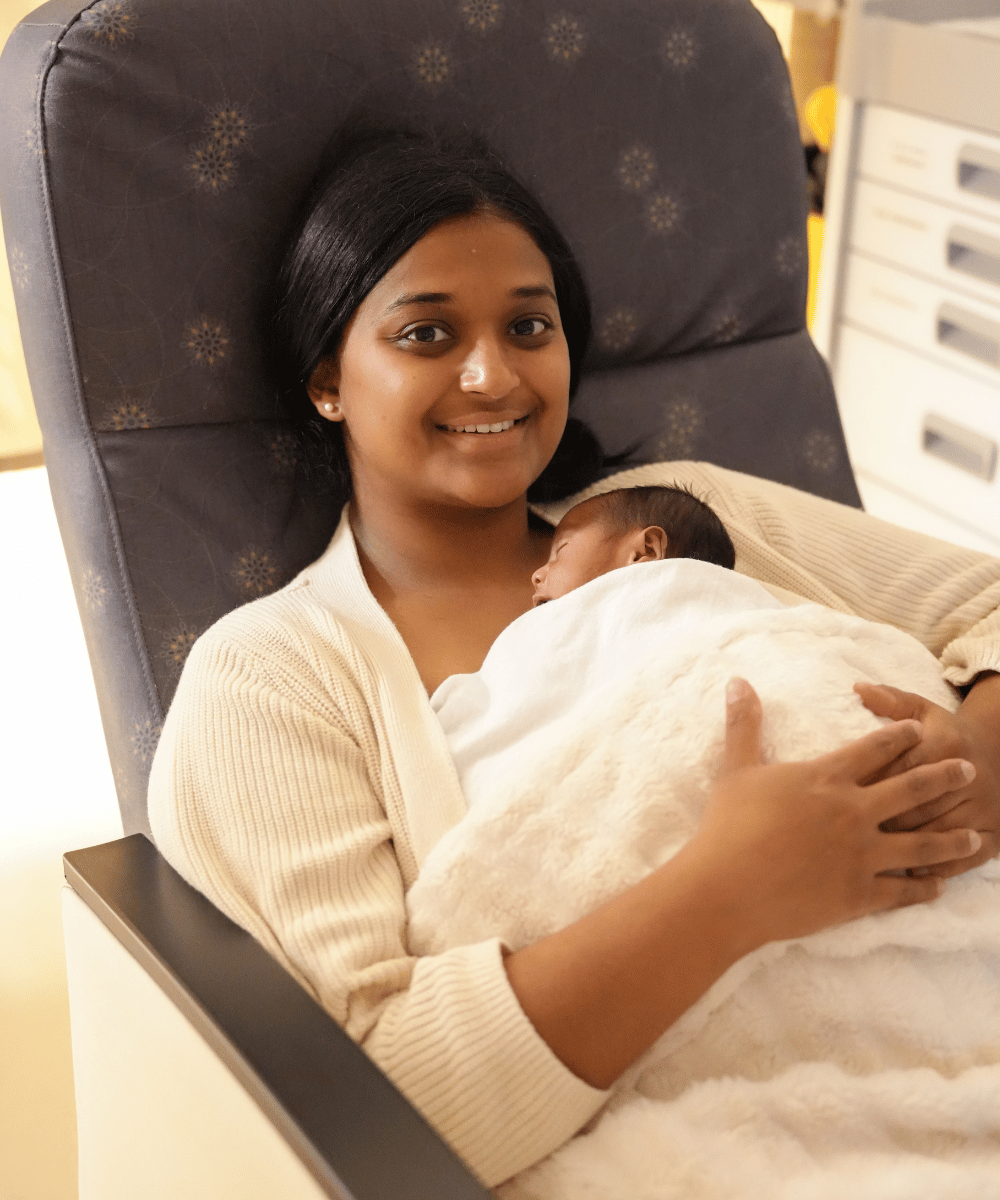
Knowing the NICU team had the best tools available helped us trust the care and focus on our baby.
Gaya Indra

Handled with care
During active labour, it became evident that Gaya’s baby was in distress. Her delivery, led by Dr. Renée Chouinard, Oak Valley Health Obstetrician/Gynaecologist, quickly shifted to an emergency caesarian section. An epidural was administered to ensure her comfort and safety.
“Dr. Chouinard made the best educated calls for my particular situation,” says Gaya.
After 12 hours of labour, baby boy Benji Indra Kathir arrived on October 14, 2025, at 32 weeks and five days, weighing just 3lbs 6oz. Despite his early arrival, he was able to breathe and cry on his own. He was immediately transferred to MSH’s Neonatal Intensive Care Unit (NICU).
The specialized care delivered by Dr. Sharma and Dr. Taslim Dawood, Oak Valley Health Neonatologist/Paediatrician, set the tone for each day that followed in the NICU. They took their time to explain the treatments Benji needed, answering any questions the concerned new parents had. The nurses in the NICU were there for the family every step of the way, too — especially for Gaya as a new mom. They supported her through many firsts and milestones during a stressful time.
“That really changed my care for Benji. I learned a lot about how to take care of him from the nurses — how to hold him, how to feed him, how to bathe him, how to pump for the first time. All tools that I use today,” she says.

Article from
Gaya Indra







.png)









.avif)



















